Design question: How might we help patients and caregivers easily understand and track their ED/ER visit status in real time, reducing anxiety and improving transparency throughout their journey?
Target users: ER patients with non-urgent needs and their caregivers
Transparent Patient Care in the ER
Timeline
10 weeks, as part of User-Centered Design course (Autumn 2025)
Team
Auli Badoni, Nicholas Murphy, Ethan Zhang
“Anxiety is amplified by uncertainty; Not knowing how long they’ll wait, what will happen next, or when they’ll receive results contributes significantly to distress and perceived poor care.” (Meloncon, 2017)
We initially began exploring this topic due to our own frustrating experiences with the lack of transparency in the ER. Our research validated that this is a systemic issue; patients often find the lack of information during their stay more distressing than the wait time itself.
This project aims to solve that uncertainty by designing better avenues for communication and transparency.
User Research
To validate our assumptions about ER frustrations, we investigated the transparency gap through patient / caregiver surveys, provider interview, and secondary research. We discovered that patient anxiety is primarily driven by uncertainty and communication breakdowns rather than the wait duration itself.
Key themes emerged regarding the critical need for transparency and education; users prioritized general progress indicators and context on why delays occur over precise but unreliable time estimates.
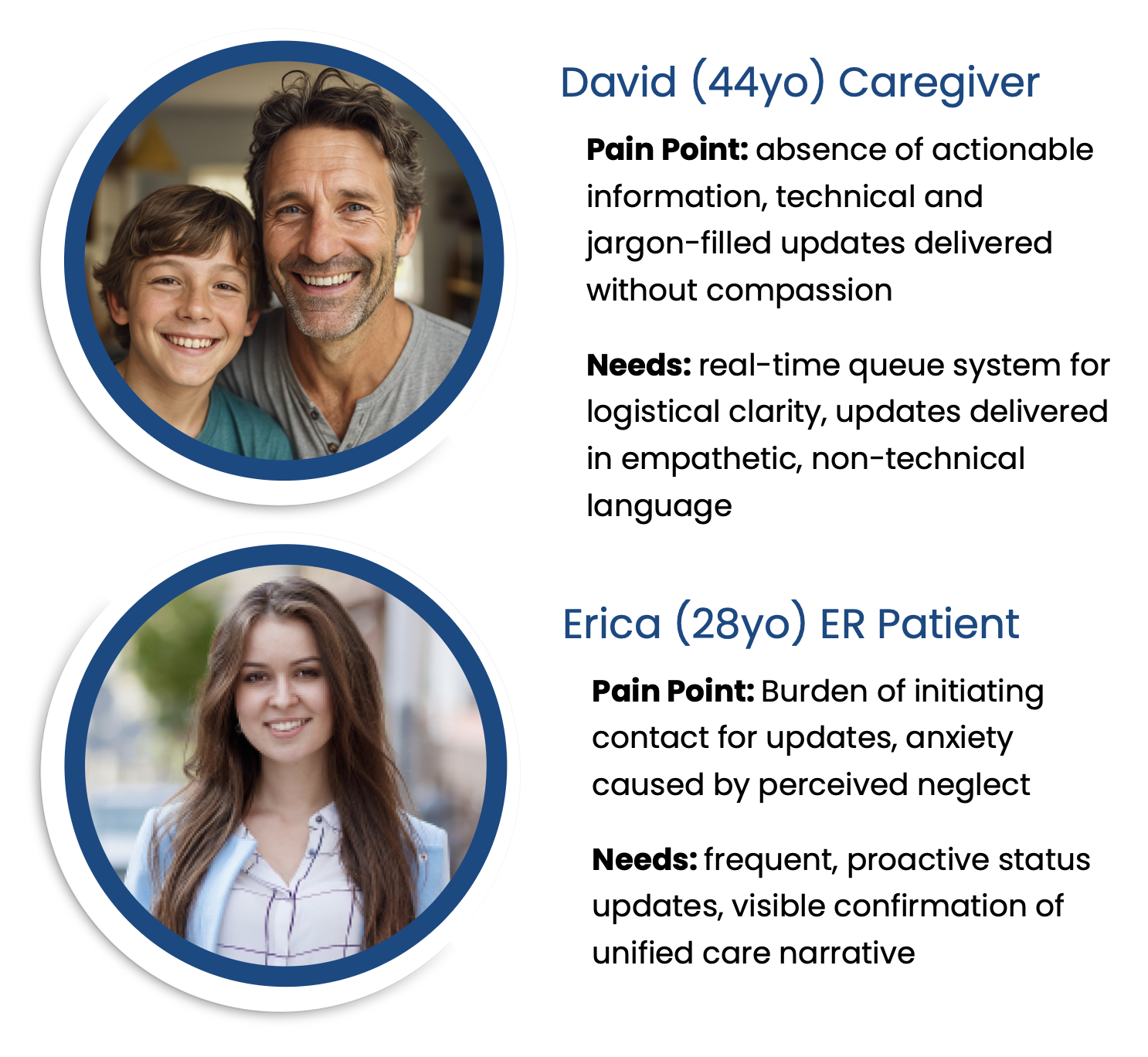
These findings confirmed the necessity of a multi-channel solution and provided the specific insights required to develop our user personas.
-
Communication: Patients frequently report communication breakdowns and inadequate information. Physicians often focus solely on physical illness, lacking empathy (Roh & Park, 2016).
Anxiety & Uncertainty: Patient stress is largely rooted in the uncertainty of wait times, next steps, and when test results will arrive (Ehrler et al., 2016; Meloncon, 2017).
Lack of Transparency: Patients feel forgotten during long waits, especially without updates on wait times, delays, or test results (Manukumar et al., 2025).
Information Need: Overwhelmingly, patients want wait times posted (90.8%) and believe it would improve satisfaction (76.7%) (Mohseni et al., 2021). They also desire access to and control over their medical records (Esmaeilzadeh, 2019).
-
A Google Forms survey was distributed to collect quantitative and qualitative data from 40 participants: (40% patients, 57.5% caregivers).
40% of participants rated their ED/ER experience as neutral (3/5).
35% confirmed that status uncertainty increased stress, validating secondary research.
57.5% believe a progress indicator would help.
85% prefer in-person verbal updates, followed by app/text updates (42.5%).
Validated the need to explain the "broader ecosystem" (why delays occur) to manage expectations.
Confirmed a strong need for explanations in "layman's terms," avoiding medical jargon.
-
The "wealth of 'I don't knows'" drives patient frustration. Providers struggle to give specific time estimates ("If I tell you a certain time... I'm a liar") due to the unpredictable nature of the ER.
Patients often don't understand medical explanations or why they are waiting, leading to anxiety and the feeling of being forgotten.
A significant amount of provider time is spent fielding repetitive status requests from families.
A real-time status tracker (via mobile) would be helpful for visualizing progress and confirming the patient hasn't been forgotten.
Some nurses use QR codes or "Badge Buddies" to provide layman's explanations of the care process.
In-room tablets could be useful for non-tech-savvy patients who cannot use personal smartphones, potentially activated via wristband scanning.
Success depends on managing patient expectations.
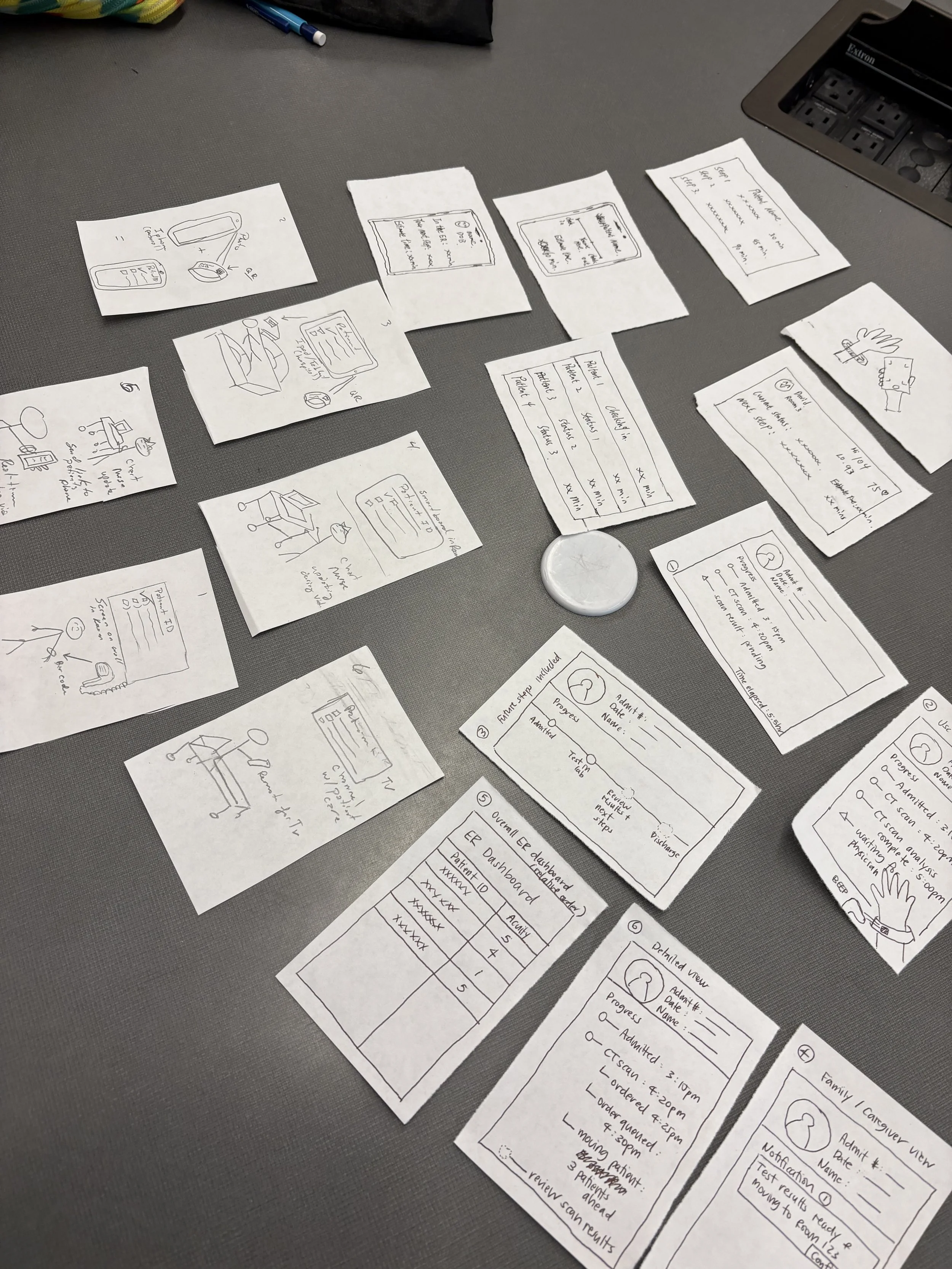
Ideation
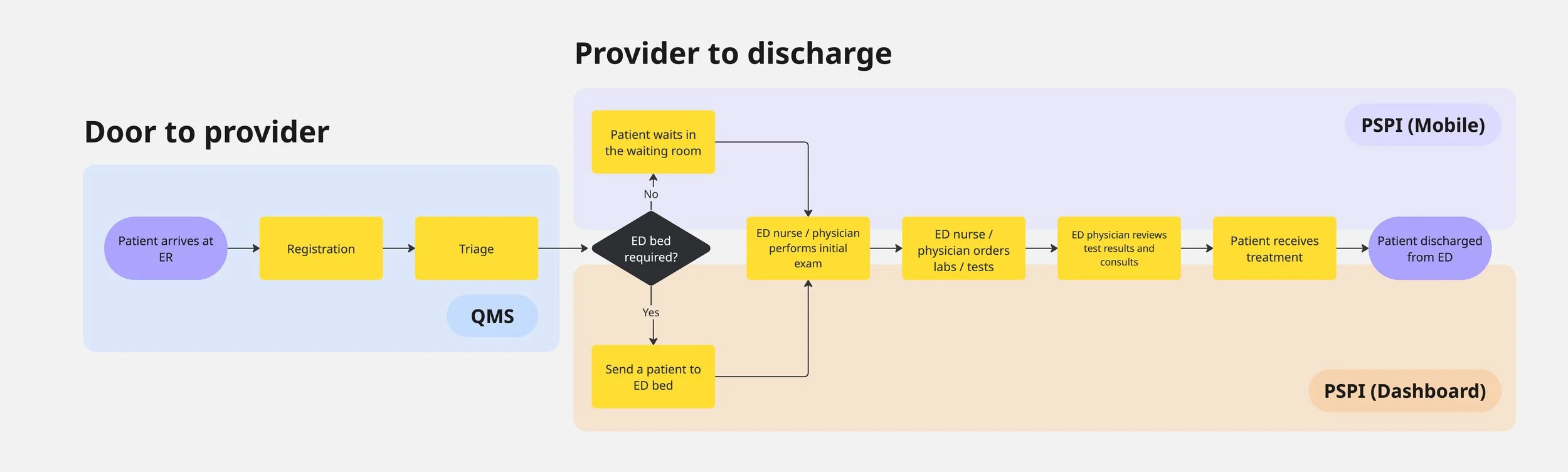
Building on our research insights, we brainstormed and sketched potential solutions. We quickly realized that "wait time" is not a static event but a recurring pain point across various stages of care, which led us revise our design question and pivot from a singular feature to an integrated "door-to-discharge" system.
This exercise helped us map a comprehensive user flow that accounts for distinct constraints, such as bed assignments and multiple touchpoints, establishing the structural framework needed for defining a user flow and designing prototypes.
User Flow
Revised Design Question 🔎
How might we design an integrated Queue Management System (QMS) and Patient Status and Progress Indicator (PSPI) system leveraging existing hospital technology (i.e., medical band and electronic health records)?
Prototypes
We developed high-fidelity prototypes through multiple rounds of iteration, incorporating feedback from initial usability testing to better serve our user personas.
Key enhancements include:
Adding estimated wait times alongside timestamps
Translating medical status updates into plain language within the Patient Status Progress Indicator (PSPI)
Clarifying queue hierarchy in the Queue Management System (QMS)
Queue Management System (QMS)
A public waiting room display that visualizes the triage queue using tokenized patient IDs to ensure HIPAA compliance, clearly indicating queue position while protecting personal identity.
PSPI (Mobile View)
A portable companion interface that ensures patients and caregivers have access to critical progress updates and notifications even when stepping away from the bedside.
PSPI (In-room Display)
A bedside monitor accessed via the QR code on the patient’s medical wristband, providing a secure, personalized view of their care journey with real-time status updates and estimated wait times.
Next steps
Validating the system with medical professionals to ensure clinical feasibility and address provider pain points